I think it’s safe to say that we’re all fairly familiar with our five senses: seeing, hearing, touching, tasting, and smelling. But what self-respecting etymology blog calls it a day with those terms? We need to be more rigorous!
sight → vision → Latin, videre (to see)
hearing → audition → Latin, audire (to hear)
touch → taction → Latin, tangere (to touch)
taste → gustation → Latin, gustare (to taste)
smell → olfaction → Latin, olfacere (to smell)
There are even fancier terms for these, such as ophthalmoception, but let’s not get too carried away.
Ophthalmoception
Origin: Neo-Latin, ophthalmos (Gk. eye) + recipere (L. to receive)
To receive from the eye, i.e., vision
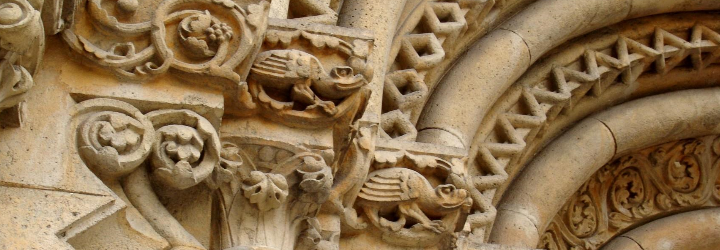
The Sense of Sight and Smell, by Brueghel the Elder
Without getting into fantastical and/or esoteric discussions of the legendary sixth sense, it turns out that we have much more than five senses. These “nontraditional senses” depend on special receptors in our bodies, and some of them don’t rely on specific sensory apparatus (singular: apparatus) (no, that’s not a joke). One classic example is proprioception, which is the ability to know where one’s body is in three-dimensional space. Unconscious proprioception relies on the cerebellum, whereas conscious proprioception relies on the dorsal column/medial lemniscus (DCML) tract to the parietal lobe.
Proprioception
Origin: Latin, proprius (one’s own) + -recipere (to receive)
To receive one’s own, i.e., information about one’s own body
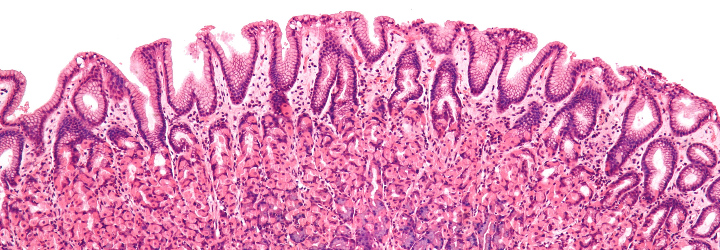
What about the sensation of pain? Pain is a complex topic and much research has gone into it. Our current understanding of pain is that pain is not directly sensed by the body; rather, it is “interpreted” by the body after exposure to a noxious stimulus. Noxious stimuli stimulate peripheral nerves and the central nervous system generates pain. The detection of noxious stimuli is done via nociception by nociceptors.
Nociception
Origin: Latin, nocere (to hurt/harm) + recipere (to receive)
To receive hurting/harm, taken to mean pain
Again, rigorously, our bodies to do not directly sense pain—they sense noxious stimuli, and develop pain in response. Also note that it is difficult to assign a definition to pain, for it is a subjective phenomenon: we all respond to noxious stimuli differently.
Descartes thought that animals lacked consciousness—and thus could not feel pain
I was given a request for the adjective forms of some of the nontraditional senses, but I couldn’t find many of them in any dictionaries. I did find the adjective form for proprioception: proprioceptive. Using this convention, here is a list of adjectives:
proprioception → proprioceptive
nociception → nociceptive
chronoception → chronoceptive
thermoception → thermoceptive
I haven’t discussed the last two terms on this list; what are their etymologies? Leave a comment below with your answer!