Animals were of prime importance in the classical world: agriculture in the Roman Empire depended on domesticated oxen (L., bos) to plow the fields, crowds of thousands cheered on the races at the Circus Maximus, as drivers atop their chariots urged on the fastest horses (L., equus) in the land, and sacrifices of sheep (L., ovis), and pigs (L., porcus) were necessary to please the gods. So too were animals important to ancient scientists and physicians. It was the dissection of and the experiments on animals that formed the basis for early understanding of human anatomy and physiology. In addition, there are countless anatomic terms whose etymologies derive from the Greek and Latin names of animals.
Cauda equina
Origin: Latin, cauda (tail) + equus (horse)
Horse’s tail
Sitting within and protected by the vertebral column, the spinal cord consists of nerve cells and their extensive myelinated tracts that carry motor, sensory, and autonomic data to and from the brain. One would think that the spinal cord extends all the way to the bottom of the vertebral column, but in fact it stops looking like a cord at the level of the L2 vertebra in adults. At that point, it gives rise to the so-called cauda equina where individual nerves arising from the lower part of the spinal cord descend down the vertebral column until they exit through the proper foramina. It’s no wonder then why lumbar punctures must be done below L2: the individual nerves of the cauda equina can easily accommodate the lumbar puncture needle unlike the large-diameter spinal cord. So the next time you consent a patient for an LP, be sure to ask yea or neigh.
Coccyx
Origin: Greek, kokkux (cuckoo)
The vertebral column consists of seven cervical, twelve thoracic, and five lumbar vertebrae. The primary role of these bones is to protect the spinal cord. However, their articulations allow flexion, extension, lateral motion, and rotation of the back, explaining their derivation from vertere (L., to turn). There are two more bones that lie below L5. The sacrum, which the Romans called the os sacrum (L., sacred bone) and which the Greeks named the hieron osteon (Gk., sacred bone), sits within the pelvis and allows the sacral nerves of the cauda equina to exit through its foramina. It’s not clear why this bone was considered “sacred.” One thought is that its sacredness derives from its location in the pelvis and therefore an association with reproduction. Another theory suggests that the ancients used this bone during sacrificial ceremonies. Finally, below the sacrum sits the coccyx, the small bony remnant of a vestigial tail. The ancient anatomists who named this bone thought that, when viewed from its side, it bears resemblance to a cuckoo’s beak.
Tragus
Origin: Greek, tragos (goat)
The tragus is that small piece of cartilaginous tissue situated next to the opening of the ear canal. And for some strange reason, it’s derived from the Greek word for goat. Perhaps some Greek anatomist had particularly hairy ears and thought it resembled the hair on a goat’s chin. Whatever the reason, the association with goats definitely stuck: the medical term describing hair on the ears is barbula hirci, literally meaning “little beard of the goat” [L., barbus (beard) + hircus (goat)]. No kidding.
Concha
Origin: Greek, konkhe (mussel, shell)
Within the nose lie the superior, middle, and inferior nasal conchae. These long shelves of bone on the lateral aspects of the nasal cavity are covered with mucosa and supplied by a rich network of blood vessels. Their most important function is to warm and humidify the air as it passes from the nasal cavity to the lungs. If I look really hard, I can make myself believe they look like little mussels. Astute readers will notice that concha also appears in the labeled anatomy of the outer ear: concha also describes the fossa next to the opening to the ear canal.
Pes Anserinus
Origin: Latin, pes (foot) + anser (goose)
Goose’s foot
Three muscles of the leg, the gracilis [L., gracilis (slender)], sartorius [L., sartor (tailor)], and semitendinosus [L., semi (half) + tendere (to stretch)], give rise to tendons that travel in parallel before attaching to the same location on the tibia. The ancient anatomists who saw this arrangement must have been reminded of the tripartite webbed feet of the goose and named it as such. There is a clinical condition called “pes anserinus pain syndrome,” also known as “pes anserine bursitis,” that describes pain around these tendons on the medial side of the knee. Interestingly enough, pes anserinus is not only a structure in the leg: it also is another name for the parotid plexus, where the facial nerve branches after exiting the stylomastoid foramen.
Recurrent Laryngeal Nerve
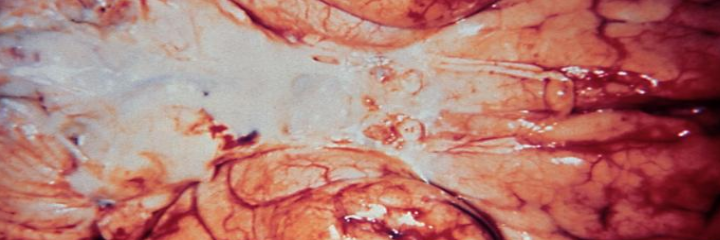
Galen demonstrating the effects of the recurrent laryngeal nerve during the dissection of a pig
The recurrent laryngeal nerves are branches of the vagus nerves that control nearly all of the intrinsic muscles of the voice box. Therefore, injury to one or both may cause hoarseness or even a complete inability to phonate. The etymology is nothing to write home about, but the story of their discovery definitely is. The famed Greek physician Galen, while conducting an experiment on a live, strapped-down pig, accidentally cut both laryngeal nerves; the pig continued to struggle but completely stopped squealing. He ultimately traced out the path of the nerves and confirmed that they originated from the vagus nerves. He noted that “there is a hairlike pair [of nerves] in the muscles of the larynx on both left and right, which if ligated or cut render the animal speechless without damaging either its life or functional activity.” Galen held a public demonstration of his experiment in Rome that was well-attended by distinguished politicians and scholars of the time. Those readers interested in learning more can read the article “Galen and the Squealing Pig,” linked here.
Thanks for taking a trip to the zoo with me. I’m off to see the capybara exhibit.
P.S.: Can you think of the English adjectives derived from the Latin words mentioned in the first paragraph? As a bonus, what about the adjective that describe wolves? Fish? Ducks?