In the medical field, there is a consistent misuse of the words hypertrophy and hyperplasia. It’s not quite as egregious as the misuse of the suffix “-itis,” but it is still saddening—at least to me. An etymological breakdown can help us differentiate between the two terms:
Hypertrophy
Origin: Greek, hyper (over/above) + trephein (to feed)
To overfeed ; taken to mean an increase in cell size
Hyperplasia
Origin: Greek, hyper (over/above) + plassein (to mould)
To mould over; taken to mean an increase in cell number
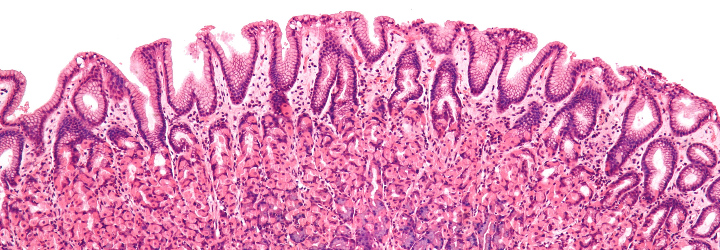
These are the definitions on the cellular level, but it turns out that some pathologists also use the term hypertrophy to denote a gross increase in organ size, hence the confusion. For example, when a man’s prostate becomes enlarged, it is due to hyperplasia (an increase in cell number). The cellular term for this phenomenon is nodular hyperplasia. On an autopsy report, however, a pathologist would report it as prostatic hypertrophy because he or she can see the increase in size through the naked eye. Hyperplasia is a normal physiological response and it is not pathologic. A good example is the hyperplasia of the uterine lining (the endometrium) in the menstrual cycle.
Note, however, that the story with hyperplasia is a bit more nuanced than that. In the case of the endometrium [Origin: Greek, endo- (in) + metron (womb)], physiologic hyperplasia is termed “simple hyperplasia without atypia.” The term simple vs. complex denotes that the cells either have or have not proliferated to the point of interfering with the normal architecture of the endometrium. The modifier of “atypia” denotes a structural abnormality of the cells; thus, atypical cells can be considered to be dysplastic.
This brings us to another pair of -plasias that is often confusing to people: neoplasia vs. dysplasia. The difference between these two terms is a bit more subtle, but again, some etymology may be of use to us.
Neoplasia
Origin: Greek, neo– (new) + plassein (to mould)
A new moulding; taken to mean an abnormal proliferation of cells (either benign or malignant)
Dysplasia
Origin: Greek, dys– (ill) + plassein (to mould)
An ill molding; taken to mean an increased number of immature cells (compared to regular cells) and greater variability between cells
On a functional basis, dysplasia may progress to neoplasia, but dysplasia by itself doesn’t denote an abnormal growth or increase in cell number. Indeed, dysplasia results in an increased ratio of immature to mature cells and variability because it has acquired just enough mutations to appear odd—hence, depending on the situation, its progression to neoplasia. One might then ask: “What about carcinoma in situ (CIS)?” Well, dear reader, CIS is a subset of neoplasia (abnormal proliferation of cells), but one that has not invaded through the basement membrane:
There are other types of “–plasias,” such as metaplasia & desmoplasia. What do you think these terms denote and where do they come from? Let me know in the comments section!